Bacterial Vaginosis (BV) is the most common vaginal infection globally, affecting women across their lifespan. Despite its prevalence—impacting about one in three women in their reproductive years—it tends to carry a stigma. BV can also be confused with other vaginal infections, due to a similarity of symptoms. This is all the more reason why we must learn and talk about BV.
FemmePharma believes your vaginal health is a pillar of your overall wellness. Let’s move past the shame, understand the biological causes of BV, and empower ourselves with the expert knowledge so we get the care we need. BV is a highly treatable disease, not a personal failure.
The Science of Our Microbiome
Bacterial Vaginosis occurs when the delicate, self-regulating ecosystem of the vagina—our vaginal microbiome—is disrupted.
For women’s health, Lactobacillus bacteria is a key player. These “good” bacteria act as our primary defense system, producing lactic acid that maintains a naturally acidic pH (typically 3.5 to 4.5). This low pH environment is essential for keeping “bad” bacteria, like Gardnerella vaginalis, in check.
BV occurs when our protective Lactobacillus levels plummet, allowing the disruptive bacteria to overgrow. Any event that alters the vaginal pH can trigger this imbalance, leading to the characteristic symptoms that one too many women are familiar with: extra vaginal discharge with an unpleasant “fishy” odor.
BV Affects Women at Every Stage
These are the most common risk factors that cause bacterial vaginosis and can disrupt women’s natural pH:
- Sexual Activity: Semen is alkaline, which temporarily raises the vaginal pH, making the environment less protective. While BV is not classified as a Sexually Transmitted Infection (STI), having multiple or new sexual partners can increase the risk of contracting it.
- Douching: Washing inside of the vagina is one of the quickest ways to eliminate protective Lactobacillus and alter vaginal pH, making the area more vulnerable to infection.: Do not douche! Use a mild soap, washing outside of your vulva. There is a reason the vagina is considered a self-cleaning system—trust your vagina.
- Hormones: Estrogen is the fuel for our Lactobacillus bacteria, maintaining the acidic environment our vaginas need. When estrogen levels decrease during perimenopause and menopause, this makes the vaginal environment less acidic and increases vulnerability to infections, like BV.
The Estrogen Factor
The risk of bacterial vaginosis increases significantly for women in the perimenopausal and postmenopausal phases. This is where estrogen loss plays a central role.
- Lactobacillus: Lactobacillus bacteria rely on estrogen to flourish. When estrogen levels decline during these life stages, vaginal tissue thins and the supply of glycogen—the necessary food source for Lactobacillus—is reduced.
- Vulnerability: As the protective bacterial shield weakens, the vaginal environment becomes less acidic and more susceptible to bacterial overgrowth. This connection is why treating underlying estrogen deficiency (Genitourinary Syndrome of Menopause, or GSM) is critical to preventing chronic recurrence of BV in older women.
Dangers of Delay
One of the biggest obstacles in treating BV is self-misdiagnosis. BV symptoms—that notable “fishy odor” and gray-white discharge—are frequently confused with yeast infections (which typically present with odorless “cottage cheese” discharge and itching).
- Treatment: There is no over the counter (OTC) treatment for BV. Using OTC yeast infection remedies when you have BV not only delays the proper treatment but further disrupts the microbiome. This may worsen BV infection and increase the risk of complications.
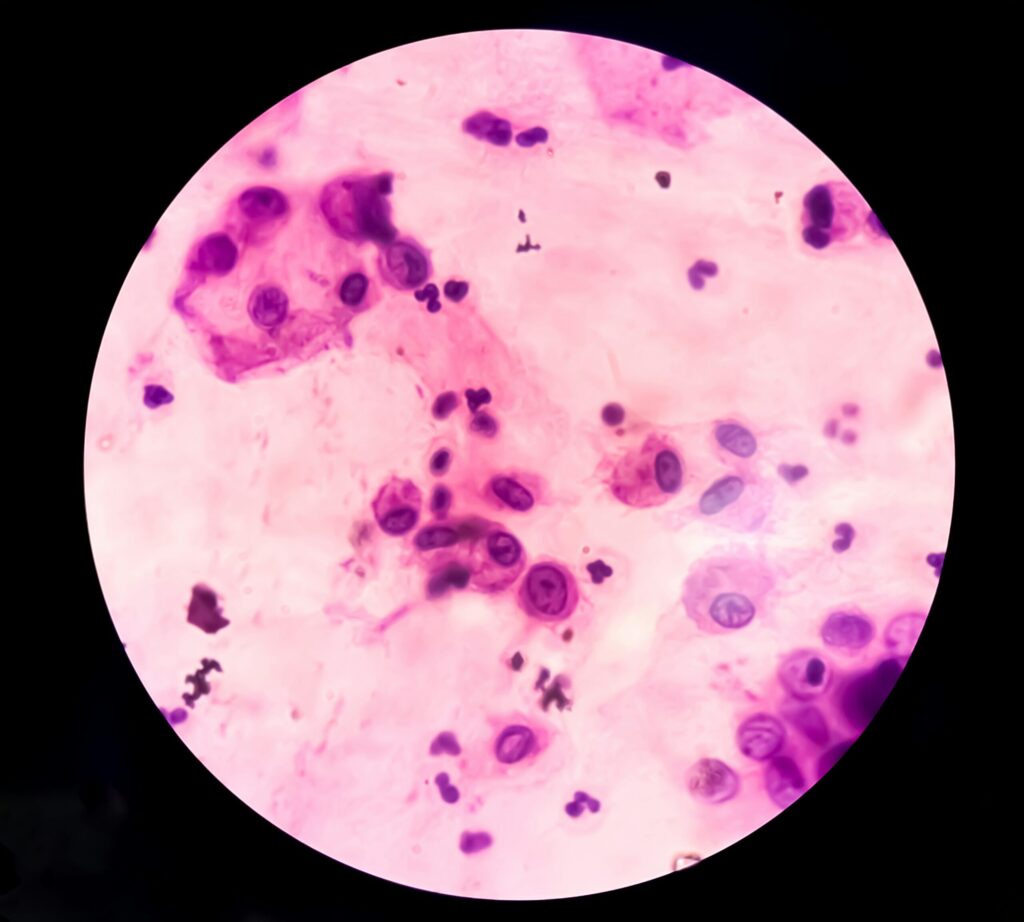
- Providers: If you think you have BV, seek a medical diagnosis. A healthcare provider uses clinical criteria (like Amsel criteria or the Nugent score) and a microscopic analysis of vaginal fluid to confirm the diagnosis. Untreated BV can increase the risk of contracting STIs and pelvic inflammatory disease (PID).
Treatment + Proactive Prevention
The first line of defense against a BV infection is a course of prescription antibiotics (oral or vaginal) prescribed by your healthcare provider. At FemmePharma, our focus is on proactive prevention and recurrence management—the long-term strategy for women’s health—so let’s explore that:
- Our Microbiome: Studies show that taking a targeted, oral women’s probiotic, like our Mia Vita Women’s Probiotic, can significantly help reduce BV recurrence. These probiotics contain the strains of Lactobacillus we need to stabilize our biome, which travel from the digestive tract to the vagina. This replenishes the good bacteria for maintaining our protective acidic pH, which keeps the BV-activating bacteria at bay.
- Hygiene: Avoid douching entirely. Use only water and fragrance-free soaps on your external vulvar area. Using condoms also reduces sperm pH disruption during sex with male partners.
- Hormones (again): If you are perimenopausal or menopausal and experience recurring BV, talk to your doctor (as Dr. Sherif advises in her chapter) about treating any underlying estrogen deficiency with low-dose vaginal estrogen. Having a healthy, thick vaginal tissue is naturally more resilient to infection.
Remember, your vaginal comfort and health are a priority at every age. By understanding the science behind the microbiome and being proactive about prevention, you may stop the cycle of BV and assume control of your wellness.
Shop FemmePharma’s Expert-Backed Intimate Wellness Solutions