Theresa Feola is making a career change. “This pandemic has given rise to re-evaluation of life on so many levels,” the physical therapist says. “For me, I finally had a moment to think.” In May, she resigned from her job to start her own business. “So The Pelvic Room is born,” she says. “The LLC is being finalized as we speak.” Operating at The Healing Sanctuary, a wellness center in Exton, Pennsylvania, The Pelvic Room is a place where women suffering with incontinence, painful sex, and pelvic organ prolapse can get therapy to rehabilitate and retrain the muscles of the pelvic floor so that they function the way they were intended.
Feola, who has been a PT for more than 30 years and is a certified pelvic rehabilitation practitioner and certified women’s health clinical specialist, calls the pelvis Grand Central Station. She calls the pelvic floor “the ultimate protector.” In other words, there’s a whole lot happening in the bony bowl defined by the hip bones, pubic bone, and sacrum. When it functions properly, it’s a thing of beauty, but when it doesn’t big problems can occur.
What is the pelvic floor?
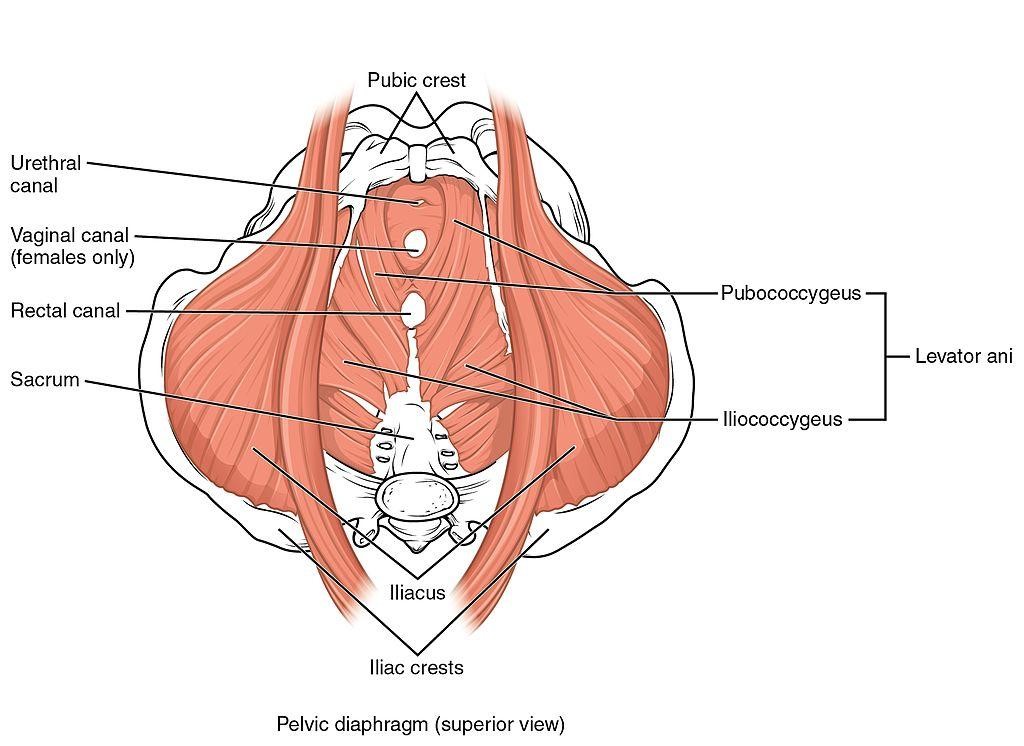
The pelvic floor is a hammock of fascia and muscle. There are two main muscles, one of which is called the levator ani. That muscle comprises three paired muscles. They all work in conjunction with the hip and abdominal muscles.
With four functions, the pelvic floor “is the start of everything,” Feola says, explaining with four S’s:
- Sphincter: bowel and bladder control
- Support: of the bladder, intestines, and uterus (if you’re a woman)
- Stability: for the lower back
- Sex: pleasure and pain
“This is your true core,” Feola says.
Exercise instructors especially use the word core a lot, she says, and assume that students know what they are talking about. But what Feola has found is that few people have an understanding of the core muscles. Few can sense or feel them working “because they are automatic muscles. They are posture muscles, just like the little spinal muscles. They are doing their thing all day long without you thinking about it, without you activating them. But we completely have the ability to improve those muscles with a little awareness.”
When there’s dysfunction of the pelvic floor — which is incredibly common and ignored more often than not — you can have problems contracting or relaxing or both, Feola says. Weakness can lead to incontinence and prolapse. Tightness can make sex painful or impossible.
Pelvic floor troubles are just as common as low back pain, the therapist says, only it’s more personal and embarrassing, and so women don’t talk about it or get treated. “I work every day to try to ease people’s comfort levels with this part of their bodies,” she says.
Why pelvic floor therapy
Simply put, pelvic floor PT is exactly like PT for any other muscle. However, because the muscles of the pelvic floor are internal and mostly unseeable, pelvic floor PT is much more intimate than that for a knee or shoulder.
It’s also much less widely recommended by physicians, though Feola says probably 90 percent of OB-GYN patients could benefit from some PT. “The first thing an orthopedic doctor will do is send someone to PT. GYNs are just not used to that,” she says.
What’s more, “the damage that happens in pregnancy and delivery is not considered an injury or a trauma. It’s the only thing that we don’t rehab,” she says with astonishment. “A football player comes in with a teeny ligament on the outside of his knee for PT in one second — we see this all the time. You strain your rotator cuff playing tennis, and you’re in PT in a second. Yet all this crucial core stability, sphincter control, everything really gets damaged and stretched and out of alignment in pregnancy or with numerous other things … and we just let it sort of heal itself. We don’t try to retrain it. We don’t try to get it back to normal.”
And when menopause rolls around, all those obstetrical injuries emerge because we gain weight, we’re not as active, we’re not as strong, and we don’t have the robust estrogen levels of our youth.
Falling estrogen is a little bit like pulling the bottom out of — well — the bottom, Feola says. “Estrogen is almost like insulation in your house, and when you’re almost suddenly without it, there is no support.”
Pregnancy and childbirth aren’t the only ways to end up with a dysfunctional pelvic floor, however. Women who have lifted a lot in their jobs, who lift heavy weights for exercise, who experience frequent constipation, or who suffer repeated or chronic respiratory illnesses that cause a lot of coughing are also at risk.
Women seek pelvic floor therapy usually when they begin to experience sudden and frequent urges to urinate or start to leak urine, when sex is very painful, or when they have pelvic organ prolapse. The International Society for Sexual Medicine states that pelvic floor PT can be a treatment for endometriosis as well.
Anatomy of a pelvic PT appointment
“I think everybody comes to pelvic PT thinking, ‘OK, you’re going to give me one little exercise for my pelvis, and I am going to be good to go and I am going to stop leaking and everything is going to be fine.’ No muscle works like that,” Feola says. “You are not going to sit in the car and do a Kegel and problem solved.”
The journal Physical Therapy describes pelvic PT as “repeated voluntary pelvic floor muscle contractions taught and supervised by a health care professional.” But contractions are only part of the work, Feola says. And once you know how to contract and relax the small muscles of the pelvic floor, physical therapy teaches you to relate that knowledge to everything you do, from sex, loading luggage into your car to lifting a grandchild to rock climbing and running.
An appointment starts with “a lot a lot a lot of talking,” Feola says. Then we just look to see how a person moves around a room in general, noting how large external muscle groups function.
“Maybe you have horrible back pain, and that’s part of what’s keeping the pelvic floor tight,” she says. “Maybe you have a hip dysfunction — hip muscles and pelvic floor muscles work together. Maybe you have an old ankle injury and you never quite got that leg to accept the weight, and so the pelvis is trying to balance you out and is working harder. Maybe your outside glute is weak and the pelvic muscles are compensating,” she says.
The next step is to look externally at the muscles of the pelvic floor and, if a client is willing, the therapist will touch the muscles, starting with those on the outside and then moving to the inside. Yes, this means that Feola places her fingers inside clients’ vaginas.
Some women are very quick to get a feel for contracting and relaxing their muscles. After that Feola may be able to help those women put that effort together with very simple exercises, and so one or two sessions are all that’s needed. Other women need six to 10 sessions before they learn to sense and recruit those muscles and then move on to putting it together with functional movement.
There are other cases, Feola says, when after a dozen sessions the patient and therapist both begin to realize that the issue a woman is experiencing isn’t a physical problem so much as a problem in her relationship or even cultural conditioning. In those cases, help from a clergy member or mental health professional may be enlisted.
The benefits of a vaginal moisturizer in pelvic PT — and life
A lubricating moisturizer is essential for successful pelvic floor PT. “We can’t get started without it,” Feola says, referring to the internal portion of her work as well as the homework that may be prescribed. “If you are going to need to use a wand or a dilator to do stretching at home, you’re going to need a lube for that,” she says.
The therapist also calls a vaginal moisturizer a no-brainer when it comes to painful sex. “That’s the very first, quickest, easiest thing that you can do to make sex more comfortable,” she says. “If there’s friction during sex, no matter how much you relax, it’s not going to feel good.”
She advises her new-mom and breastfeeding-mom clients who have vaginal dryness and pain to make things easier on themselves and help ensure a good experience by lubing up before sex. “Things are going to be so much better just by doing that alone,” she says.
Feola says, “My recommendation is a daily moisturizer (Mia Vita™ Gel) for vulvar irritation, burning, pain, itch commonly seen with my patients for a variety of reasons, such as hormonal changes; oral contraceptives; stress; vulvar hygiene habits; a chronic pain cycle, which could have started with even a simple UTI; acute/intermittent irritation post-penetration; or even friction from bike riding.
Women with pelvic organ prolapse can also really benefit from a vaginal moisturizer or lubricant. “Prolapse is a big source of vaginal tissue friction/irritation — a daily moisturizer like that from Femmepharma helps tremendously,” Feola says.
“The daily moisturizer is safe to use as needed and frequently throughout the day for comfort. Mia Vita™ Personal Lubricant & Moisturizer is used in the clinic for internal vaginal pelvic floor muscle exams and treatments. Mia Vita™ Personal Lubricant & Moisturizer is recommended for use during penetration, whether that is intercourse, with toys, or a physical therapy dilator home program.”
If you want to learn more
Pelvic floor therapy is a relatively new field, but there are a few journal articles that may interest you as you consider whether a physical therapist like Feola could benefit you.
- Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women
- Effectiveness of pelvic floor muscle training and bladder training for women with urinary incontinence in primary care: a pragmatic controlled trial
- Menopause: PTs help to ease ‘the change’
- Effect of behavioral and pelvic floor muscle therapy combined with surgery vs. surgery alone on incontinence symptoms among women with mixed urinary incontinence
- Pelvic floor physical therapy for vulvodynia
Photo: Delmaine Donson
